
Efforts to find less-invasive and more affordable cure for two common genetic disorders — beta thalassaemia and sickle cell anaemia — have received a boost with Aga Khan University’s research centre recently winning a competitive research grant of Rs159.60 million.
Currently, Pakistan has an estimated 100,000 transfusion-dependent thalassaemia patients with 5,000 babies born with the disease every year.
On the other hand, sickle-cell disease is one of the well-known causes of anaemia in the country.
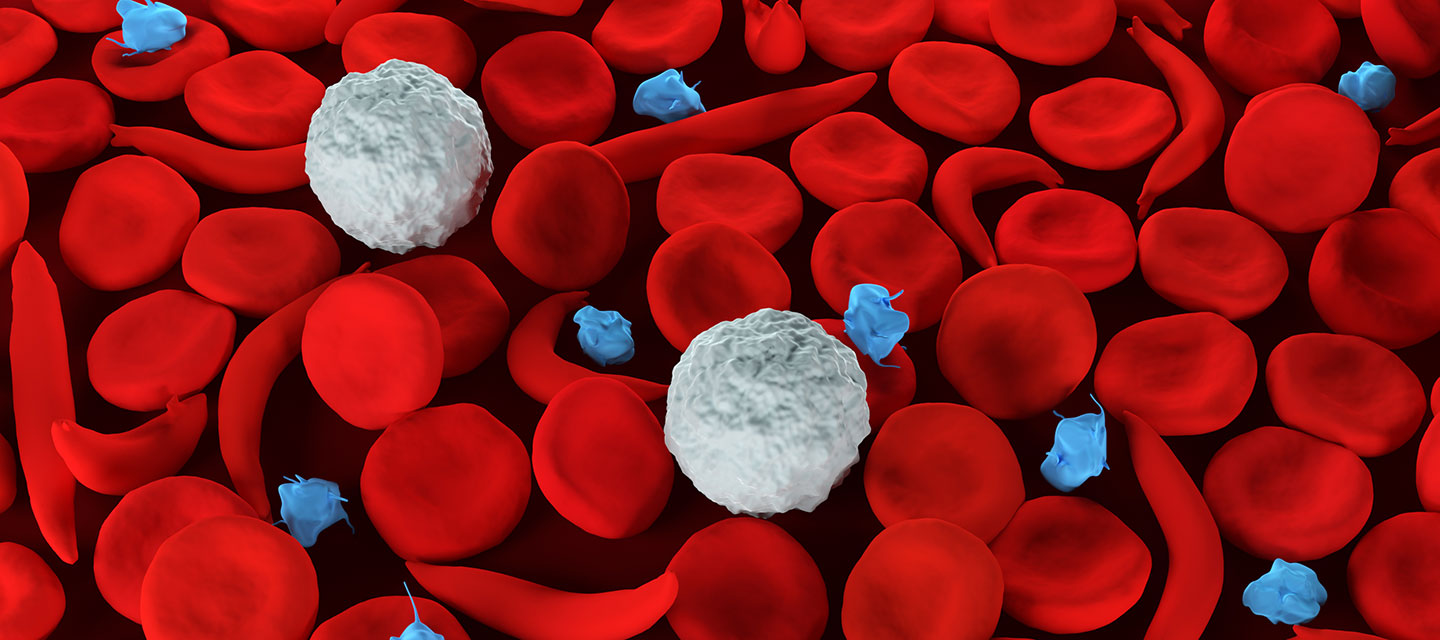
Doctors and research scientists are aware that mutations in the haemoglobin beta-globin, HBB gene causes both diseases. Patients suffer from a lack of haemoglobin, the protein that carries oxygen from the lungs to the rest of the body; and a lack of oxygen in the body’s tissues can lead to poor growth, organ damage and other health problems.
The only treatments available are blood transfusions or bone marrow transplants, both with drawbacks and side effects.
Blood transfusion often leads to iron overload and organ damage while bone marrow transplant is a costly, risky and invasive treatment available only to patients who can find suitable donors with matching blood stem cells. Also, limited bone marrow transplantation facilities and expertise within Pakistan mean that most patients cannot access this treatment.
Given these challenges, researchers around the world are looking at new gene and cell repair therapies for a treatment and potentially a cure.
“Our research aims to find an innovative, less-invasive and more affordable cure for these common genetic diseases,” explained Dr Afsar Mian of AKU’s Centre for Regenerative Medicine and Stem Cell Research (CRM), which will carry out the study.
“Our team will be among the few researchers around the globe who are working on developing this gene editing approach. Better still, conducting this study in Pakistan will help build local capacity and solutions, instead of waiting for treatments from elsewhere.”
The team will work on gene-silencing, using the same gene editing tool and approach, suppressing the BCL11A gene that stops foetal haemoglobin from being produced.
The concepts will first be tested in the laboratory, using stem cells that have the potential to form any cell type in the body, drawn from thalassaemia and sickle-cell patients. If successful, this will be followed by pre-clinical trials to determine if the treatment is safe.
“This potential therapy could provide a permanent cure, bypassing the need for bone marrow transplant and blood transfusion,” said Professor El-Nasir Lalani, founding director of CRM.
The study team includes Drs Afsar Mian, Salma Jahan, Hammad Hassan and Mohammed Yusuf from CRM and international collaborators from the University of California, San Francisco, the Norwegian University of Science and Technology and Cardiff University in the UK.
The World Bank-supported HEC Grand Challenge Fund, launched in 2020, aims to promote research excellence in strategic sectors with awards based on competitive, peer-reviewed evaluation of proposals. CRM is one of the five winning recipients, out of more than 700 applicants in the fund’s inaugural round.
![]()





