Since the emergence of Covid-19 pandemic, multiple questions have been lingering in the minds of people. Can mankind together eliminate this deadly virus? Can we save lives and make this world a normal place to live once again? Can we regain control in a shorter time?
The answers are all hidden inside the 13 vaccines, which the scientists are looking up to, like a bunch of anxious hawks to determine which vaccine will pick up and destroy its prey efficiently. Normally, vaccines take 10-15 years to develop, but vaccine development against Covid-2 is going at a very fast pace. The whole process of vaccine development starting from SARS- COV-1 to SARS- COV-2 has been shortened and quite fast-tracked. While SARS- Covid -2 is a new virus, its exact correlation of protection is not completely defined, but there are precedents from other respiratory infections that have played a pivotal role in helping manufacture the vaccine for this new deadly strain virus.
The immune response of SARS-COV-1 was compared with SARS-COV-2 under the speculation of T-cell response which are the immune cells that recognize specific foreign particles rather than an antigen. (A substance that initiates an immune response present on the outside of a pathogen). The response of T-cells is important in the control of respiratory infections. Experiments on many animal models were carried out and it was seen that T-cells can be protective. There are many types of T-cells, such as circulating follicular T-helper cells, CD4+ T-cells, T-memory cells (CD4+ CD8+) all having different roles. It was seen in SARS-COV-1 that the T-cell memory can be long-lived as they were detected 4 years after the infection, however, their depletion in mouse models showed delayed viral clearance and enhanced disease in SARS- COV-1. For SARS- C0V-2, a similar response was seen where the T-cells were present in individuals having asymptomatic or mild covid-19 but had fewer T-cells than the healthy controls.

Comparing the antibody response of SARS-Covid-1 against Sars-Covid-2, it was demonstrated that SARS-Covid 1 antibody response was short-lived somewhat like SARS- Covid-2 As in the development of vaccines, antibodies are the backbone to impart vaccine-induced protection. It was seen by the scientists that the antibody response, particularly of IgA and IgM lasted six months only and this is expected to be possibly the same for SARS- COV-2. IgM is the first antibody that the body makes to fight the new infection and IgA helps to fight off the sickness. Several studies were carried out to understand the antibody response to SARS- Covid 2 while taking the SARS-COV-1 AND MERS-COV-2 example as a standard and comparing and visualizing their antibody response with SARS-COV-2. A delayed antibody response was found with an increase in the severity of diseases for both of the previous viruses. As for COV-2, it was found that rarely any antibodies were discovered in the first 7 days of infection, but the amount increased in the second-and third-week post-infection mimicking with its family.
To combat the disease, a wide range of vaccine approaches have been proposed, including the traditional approaches-inactivated, live attenuated, protein adjuvant, and more novel but yet unlicensed, such as viral vectors and nucleic acids. Scientists first understood the mechanism to target the virus based on the experience of SARS-COV-1. Most of the vaccines target the SARS-COV-2 spike proteins. Within the spike a receptor biding domain is present that allows the virus to enter the host cell and then targets the neutralizing antibodies. Thus, scientists are including this region in the vaccines. But since coronavirus spike is a type 1 fusion protein that is metastable undergoing irreversible conformational changes, this makes so many vaccines being ineffective as the neutralizing antibodies fail to neutralize the toxic effects of the virus.
Thus, scientists from all over the globe are working together to fight the pandemic and designed some of the vaccines as discussed below.
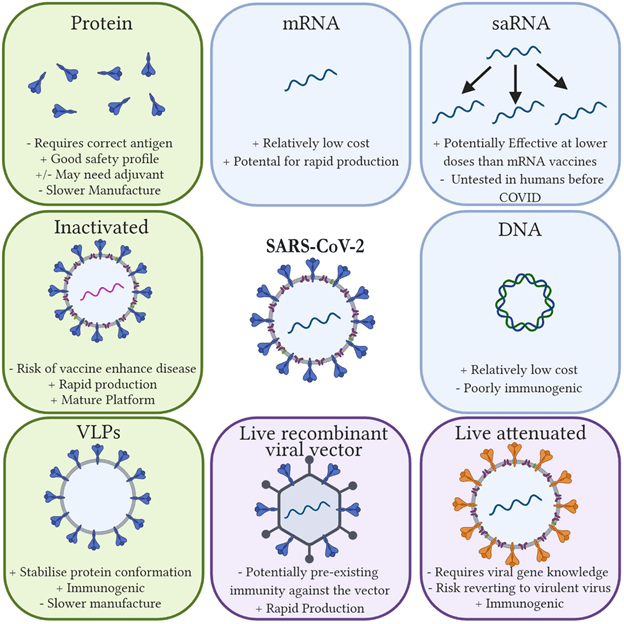
Protein Vaccines
With other pathogens, recombinantly produced viral surface proteins can be used. These vaccines have a good safety profile and low levels of immunogenicity which means they require adjuvant to improve their efficacy. Adjuvants are substances used to enhance an immune response and, therefore, improve the effectiveness of vaccine They are made by cloning the genes for the chosen antigens, then expressed and purified in the bacteria, yeast, and mammalian cells. For SARS-COV-2, eight vaccines are in trial, two of which to be announced, are from clover Biopharmaceutical and the University of Queensland.
Nanoparticle and Virus-like particle (VLP)
The VLPs are a subset of protein vaccines which are artificially produced nanoparticles and resemble virus. Proteins are taken from the viral capsid (a protein shell of a virus). On the surface of the viral capsid, several proteins are present called as capsid proteins. The purpose of the viral capsid is to enclose the genetic material of viruses. These surface proteins are taken and virus like particles are made. The vaccine produces a strong cellular and humoral response. Humoral response refers to the prevention of subsequent reinfection while cellular response refers to the immune cell’s response such as T-cells that provide immunity. The VLP nanoparticles can self-assemble. Novax has developed a recombinant nanoparticle vaccine using a baculovirus. Another company Medicago used plant NICOTIANA Benthamian to produce VLP but is still in a clinical trial.
Peptide vaccines
These vaccines are based on a peptide sequence which is the sequence of amino acids that forms a protein. A minimal immunogenic (that initiates an immune response) peptide sequence is selected that can induce the T-cell response. The peptides vaccines are produced synthetically and mimic the naturally occurring proteins of pathogens. However, instead of using an entire protein a small part or fraction of protein is taken, called epitope (which is a part of an antigen) that is recognized by immune systems and antibodies bind to it. The selection of epitopes will provide broad-spectrum immunity against multiple strains of a pathogen. These peptides are easier to produce than whole antigens. Covax has registered a phase 1 clinical trial for a multi-epitope peptide vaccine.
Inactivated vaccines
A virus is isolated and inactivated historically with any chemical agent called formaldehyde. There are four inactivated vaccine candidates in clinical trials. Sinovac, and Biotech companies have used the same platform that was SARS-COV-1. The vaccine was tested on rhesus macaques and gave complete protection for SARS-COV-2 as well as no virus was detected in the lungs. The vaccine is also made by the Sino pharm company. Here, antibody production was seen in the 2nd dose. Bharat biotech and the Institute of Medical Biology/Chinese Academy of Medical Sciences are running clinical trials of inactivated vaccines.
Live attenuated vaccines
These vaccines resemble natural infection, and a single dose is enough for the treatment. The viruses are weakened by reverse genetics, meaning, introducing mutations into genes that are virulent, in order to make them non-virulent. This method requires the identification of genes that would weaken the viral replication as well as the mutation that is inserted, which should be stable. CODAGENIX and Serum Institute of India is developing these vaccines.
Vectored Vaccines
Viral vectors, such as adenovirus, modified vaccinia virus Ankara (MVA) are used. The gene of interest is expressed from other microorganisms such as bacteria, and viruses in the vectors. Vectors cannot replicate themselves. Five non replicating viral vectored vaccines are in clinical trials. All are based around adenoviral vectors.
The University of Oxford is developing a chimpanzee vaccine vector that has entered phase 1 trials. It reduced the viral load and pneumonia when challenged with SARS-COV-2 in mice and pigs. For humans, no adverse effects were found as with only a single dose, 91% of participants had neutralizing antibody and 100% after two doses.
Nucleic acid -Vaccines
These are now on the run due to their low cost and rapid development. They use either the plasmid RNA or DNA that encodes a target antigen. Once the vaccine is delivered to the patient, the nucleic acid is taken by the cells after which the encoded antigen is than expressed. The antigen is recognized by the immune cells and antibodies will start to produce against it. Six RNA and four DNA vaccines are in trail.
DNA Vaccines
DNA vaccines are made from plasmids that contain prokaryotic sequences so that when the DNA is inserted into plasmid of E-coli cells, it will stably express the foreign DNA since E-Coli is a prokaryote. The DNA vaccines encode the proteins of the SARS -COV 1 and 2. For Sars-COV-1 M, N,3A, S proteins are encoded. Genexine, in South Korea (Zydus Cadila in India) and Osaka University in Japan, have initiated Phase I trials of DNA vaccines.
RNA Vaccine
RNA vaccines work on the same principle as DNA vaccines. They express the antigen in a host cell, but they are one step further from the DNA vaccines. Unlike DNA vaccines, the expression begins in the cytosol, and RNA vaccines skip the transcription step. The RNA vaccines are first to be developed for SARS-COV-2. They had not been previously developed for SARS-COV-1. Following are the six RNA vaccines in the clinical trials for SARS-COV-2: Moderna, Bio N Tech, Imperial College London, VacEquity, Global Health, and Arcturus.
Conclusion
It is still far too early to know which approach is best to control the pandemic with vaccines. Or which one will prove to be a “MIRACLE” for all the deadly strains of the virus. But let’s get back to the answers of the questions raised at the beginning. Can the mankind together eliminate this deadly virus? The answer to this is “Yes”.
Collaborative action worldwide is needed to control the virus which requires leadership and willingness by the countries to share their scientific research programs. Secondly, can we save lives and make this world a normal place to live once again? Deaths are inevitable but we can save many lives through mass vaccination programs now being offered. People who are still believing in myths and not vaccinating themselves will put their own and the life of their loved ones at stake. Lastly, can we regain control in a shorter time? While people have learned lessons from this pandemic, the new vaccines will play their role in reducing the burden of this pandemic. The next one might strike rigidly hard as the controls and measures will be different for another virus. But today the challenge may not be eliminating the virus but trying to live with it.
![]()

Biotechnology graduate, Doing Masters in Industrial Biotechnology from NUST, Currently doing research in Vaccinology. In my free time, I provide freelancing services, and I am an experienced academic writer in industrial, healthcare and plant biotechnology.